Overview
This section describes the IAR five different levels of care that are consistent with the application and understanding of the stepped care model in the Australian primary care system. The information gathered through the initial assessment is used to recommend a level of care and inform a referral decision. The levels of care do not replace individualised assessment and care - instead, they provide a framework to guide decision-making.
It is important to emphasise that the descriptions of care at each level are offered only to guide judgements about the recommended level of care. Each presenting person, parent/caregiver, and family will have unique requirements that must always take precedence in decision-making.
There are five levels of care (depicted in Fig. 4). Each level of care is differentiated based on the intensity of the mental health treatment/intervention available at each level of care. Figure 2 shows that psychosocial and community support needs may exist at any level of care, but typically increase as the mental health need increases. The availability and suitability of psychosocial and community supports is impacted by the person’s individual needs and the intake/eligibility criteria in place for such supports. For example, government funded psychosocial support programs tend to be targeted towards people with severe and/or complex mental health needs (i.e., people who tend to need IAR Level 4 or 5 mental health services).
Grouping the complex system of mental health services available in Australia into five levels is a convenient framework to think about stepped care rather than implying that there is a natural division of service types into neatly tiered categories. While some services are associated with a single level of care, most contribute to multiple levels. For example, GP mental health care can be associated with lower levels of care when it is provided in isolation, or higher levels when delivered in combination with other services or interventions (e.g., services delivered by a psychologist or psychiatrist, or multidisciplinary team).
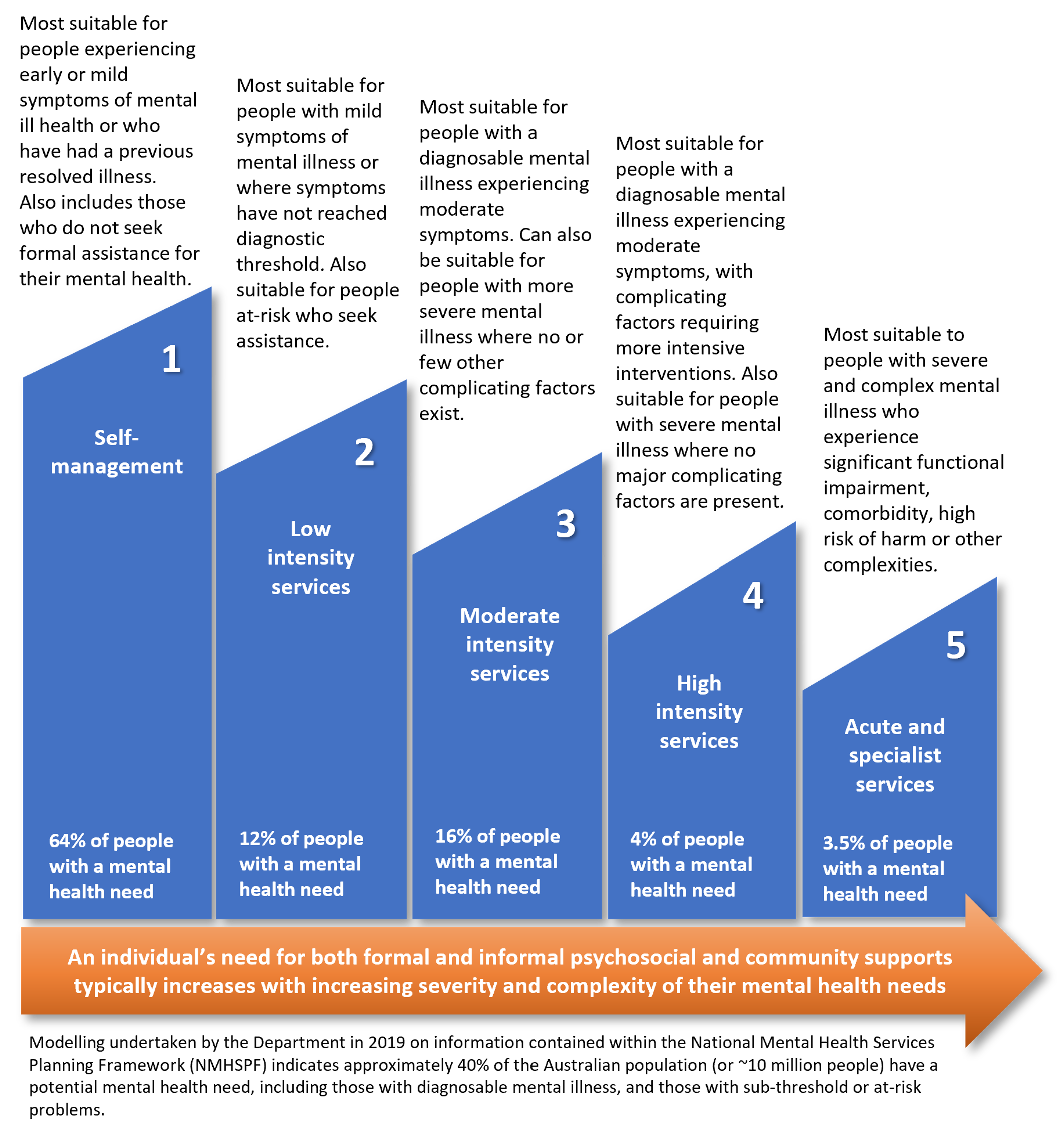
Fig. 4 The 5 IAR levels of care and mental health and community support needs
Practice Point - involving the patient and carer in decision-making
Supported decision-making strategies for initial assessment and referral:
Ensure the patient and their carer is provided with information using their preferred way of receiving information (e.g., written/verbal/visual, English/other languages, with/without a support person). Take care to provide information that is age, developmentally and culturally appropriate, particularly when engaging with children and adolescents.
Ensure the patient and their carer is provided with information about the range of services and support available (including the option of no service) and encourage the person to contribute their options, ideas, solutions, and expectations. This might include culturally important activities or self-care strategies.
Ensure the patient and their carer can express concerns or fears about the options (e.g., cost, travel, previous positive or negative experiences).
Be prepared to discuss each option’s pros and cons (e.g., intensity, length of service engagement, commitment required, waiting periods, and the potential impact on symptoms).
Check-in/follow-up to ensure the patient and their carer understands the information provided and ensure enough time for any questions.